Choosing Between Pills and Push-Ups: The New Weight-Loss Dilemma in America
In recent times, we’ve observed a significant trend in healthcare, especially concerning weight management. Millions of Americans are now opting for weight-loss drugs as their primary strategy for losing weight, rather than traditional methods like gym memberships. This shift raises several critical points worth discussing from our primary care doctors’ perspective.
Understanding the Trend
First, it’s essential to understand why this trend is occurring. Weight-loss medications have become more accessible and are perceived as a quick fix compared to the time and effort required for regular exercise. Furthermore, the pandemic has undoubtedly played a role, with many people finding it challenging to maintain a regular gym routine due to restrictions and personal safety concerns.
The Role of Weight-Loss Drugs
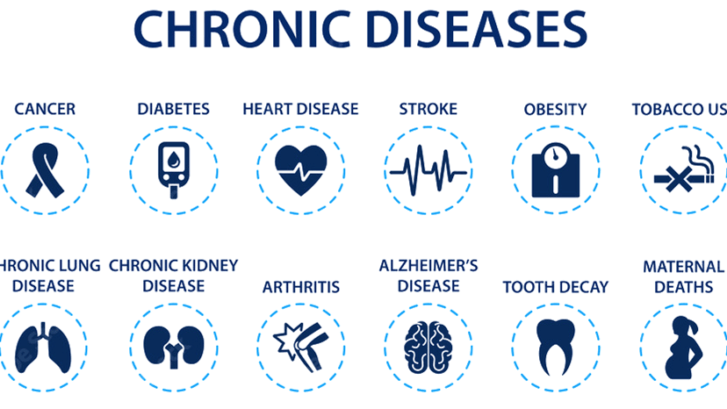
As healthcare providers, we acknowledge the potential benefits of weight-loss drugs. They can be particularly effective for patients with certain health conditions, such as obesity-related comorbidities, where losing weight is crucial for improving overall health. When used correctly and under medical supervision, these medications can offer significant benefits.
The Importance of Holistic Health
However, it’s crucial to emphasize the importance of holistic health. Weight-loss drugs can aid in reducing body weight, but they do not necessarily improve all aspects of health. Physical exercise, on the other hand, not only aids in weight management but also improves cardiovascular health, mental health, and overall physical fitness.
The Role of Primary Care
In our practice, we advocate for a balanced approach. When a patient expresses interest in weight-loss drugs, we ensure a thorough evaluation. This evaluation includes understanding their medical history, current health status, and lifestyle. We also emphasize the importance of incorporating healthy eating habits and regular physical activity into their routine.
Educating Patients
Education plays a vital role. We inform our patients about the potential side effects of weight-loss drugs and the importance of using them as part of a broader lifestyle change. It’s not just about the medication; it’s about developing a sustainable, healthy lifestyle.
Collaborative Healthcare
We also collaborate with other healthcare professionals, such as dietitians and fitness experts, to provide a comprehensive weight management plan. This team approach ensures that our patients receive the best possible care tailored to their individual needs.
Conclusion
The preference for weight-loss drugs over gym memberships is a complex issue. As primary care providers, we strive to guide our patients toward making informed decisions that best suit their health goals. It’s about finding the right balance and ensuring that the journey towards weight loss is healthy, sustainable, and beneficial in the long term.