PRIMARY CARE
At MD 2.0, we provide patients with superior primary care. We want to be the first to know about any health concerns that may arise. Primary care is performed and managed by your personal physician, Dr. Poncy or Dr. Lubarsky who are available to you 24/7.
PREVENTATIVE HEALTH
Drs. Lubarsky and Poncy believe in more than just treating you when you are sick. Our preventative medicine doctors want to ensure you are healthy year round by promoting a healthy lifestyle, yearly executive level physical exams, and helping to prevent disease.
INTERNAL MEDICINE
At MD 2.0, our concierge physician practice focuses on providing high quality care and individualized attention to each patient. Our model allows us to spend more time with each patient, allowing us to work closely with you on prevention, diagnosis, and treatment of diseases and complex illnesses.
Meet Our Doctors
Dr. Amir Lubarsky
Board Certified Internist in Jupiter, FL
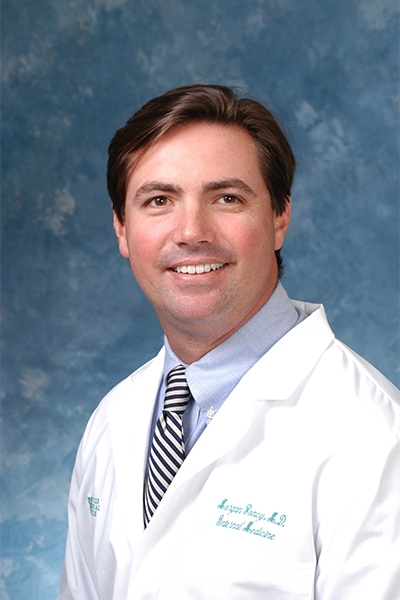
Dr. Amir Lubarsky's love of medicine allows him to listen compassionately and intently to his patients in order to provide the best outcomes.Dr. Morgan Poncy
Board Certified Internal Medicine Doctor in Jupiter, FL
Dr. Morgan Poncy is a board certified internist who was raised in the Jupiter area.LATEST NEWS

Combat Sitting: How to Stay Active and Healthy
In today's fast-paced world, many spend long hours sitting, whether at a desk, commuting, or relaxing at home. As your primary care doctors in Jupiter, Florida, we want to help you understand the health risks of prolonged sitting and how to counteract them with regular exercise.
Health Risks of Prolonged Sitting
Extended sitting can lead to several health issues, including:
- Heart Disease: Increased risk of heart disease and stroke.
- Obesity: A slower metabolism can lead to weight gain.
- Diabetes: Impaired blood sugar regulation increases diabetes risk.
- Back and Neck Pain: Poor posture and musculoskeletal issues.
Recommended Exercise to Offset Sitting
Balancing sedentary periods with physical activity is crucial. Here's what you need to know:
- Moderate Exercise: Aim for 150-300 minutes of moderate-intensity weekly aerobic activity, such as brisk walking or cycling.
- Vigorous Exercise: Alternatively, 75-150 minutes of vigorous-intensity exercise like running can be effective.
- Strength Training: Include strength training exercises at least two days a week.
- Frequent Breaks: Take short breaks every 30 minutes to stand and stretch.
Practical Tips for Staying Active
Incorporating more physical activity into your daily routine doesn’t have to be difficult. Here are some tips:
- Set a Timer: Use an alarm to remind yourself to move every 30 minutes.
- Desk Exercises: Perform simple desk exercises like leg lifts and stretches.
- Walk and Talk: Take phone calls or virtual meetings while walking.
- Active Commutes: Walk or bike to work, or park further away to increase your steps.
- Join a Fitness Class: Look for local classes in Jupiter, such as yoga or Pilates.
Our Commitment to Your Health
Our primary care office in Jupiter, Florida, is dedicated to helping you maintain a healthy lifestyle. If you have concerns about your sitting habits or need personalized exercise advice, reach out to us. Together, we can create a plan that supports your long-term health.
Remember, small changes can make a big difference. By staying active and mindful of your sitting habits, you can improve your well-being and reduce health risks. Let's take the first step towards a healthier, more active lifestyle today!

The Surge in Measles Cases: A Perspective from Our Doctors
As primary care doctors in Jupiter, it is our responsibility to stay informed about emerging health threats and provide the best care to our patients. Recently, we've observed a troubling trend in the rise of measles cases in the United States. The Centers for Disease Control and Prevention (CDC) has reported a significant increase in measles infections in 2024, with the number of cases more than tripling compared to last year.
Current Statistics and Outbreaks
As of the latest update, there have been 188 reported cases of measles in the U.S. this year, a stark contrast to the 58 cases reported in the same period last year. Outbreaks, defined as three or more related cases, account for approximately 65% of this year's infections. In 2024, we've seen 13 outbreaks compared to just four in 2023, underscoring the escalating concern.
Hospitalizations and Vaccination Status
Nearly half of the reported cases this year have necessitated hospitalization for isolation or to manage complications. This highlights the severity of measles and the critical importance of early intervention and effective management.
Alarmingly, 85% of those infected were either unvaccinated or had unknown vaccination statuses. Only a small fraction had received one or two doses of the Measles, Mumps, and Rubella (MMR) vaccine. This data reinforces the well-established medical consensus that vaccination significantly reduces the risk of contracting measles.
The Importance of Vaccination
As primary care physicians, we cannot stress enough the importance of vaccination in preventing measles. The MMR vaccine is highly effective, and the risk of contracting measles post-vaccination is extremely low. Despite the increase in cases, it is crucial to remember that vaccination remains our best defense against this highly contagious and potentially deadly disease.
Understanding Measles
Measles is an airborne disease characterized by high fever, malaise, cough, coryza, conjunctivitis, followed by a distinctive rash. It can lead to severe complications, particularly in children, and can be fatal. Given its highly contagious nature, it is imperative to maintain high vaccination coverage to prevent outbreaks.
Reflecting on Historical Data
While the current surge is concerning, it is important to put it into perspective. The number of cases in 2024, although higher than in 2023, is still significantly lower than the almost 1,300 cases reported in 2019. This comparison serves as a reminder of the importance of ongoing vigilance and vaccination efforts.
Conclusion
As primary care doctors, we urge our patients and the public to stay informed and take proactive steps to protect themselves and their communities. Vaccination is a critical component of public health, and ensuring widespread coverage is essential in preventing future outbreaks. We remain committed to providing the best care and advice to keep our communities safe and healthy.
My husband and I have been patients of Dr. Poncy for over ten years and have been extremely pleased and happy for him. He is not only a brilliant internist, but also a wonderful person. Now that he and his partner, Dr. Lubarsky, have opened the concierge practice it is better than ever. The nursing staff is superlative as is the front office staff. The office is very well appointed and comfortable. We feel very fortunate to have such a competent and caring physician.
About 11 years ago, I first met with Dr. Poncy. I came away from my appointment with him confident he understood my problem and contributed some thoughtful suggestions. Over the years, he has never changed. The outstanding staff Dr. Poncy has put together, along with his partner, Dr. Lubarsky, are the best! I honestly feel, when I have an appointment, it is like visiting "family".
I recommend Dr Lubarsky emphatically. He is a true professional: thorough, compassionate and an excellent diagnostician!
We have been concierge members for only 6 months but so far we have been very pleased. The office atmosphere is very relaxed and the doctor is able to give us the time we need. Time in the waiting room is minimal and we have been able to obtain spur of the moment appointments with no difficulty. We are happy that we joined
The new practice has a very warm, friendly, feeling to it. We don't have long waiting times. Everyone is very prompt.
I have been a patient for over 30 years. I actually look forwarded to a visit. Pleasant, professional in every way, I consider myself very lucky.
A great Dr. & great staff, minimum wait time. Spends as much time with you as you need. Same day appointments.
Dr. Poncy has been my primary care doctor for over 8 years. I've known Dr. Poncy for over 8 years. My neighbor recommended him for my diabetes and heart problem. The staff at Dr. Poncy's office is always very pleasant and Dr. Poncy is very patient to my concerns.
I have been a patient of Dr. Lubarsky since 2004. He has been such a great physician to me and my wife for several years. Recently, I was hospitalized at Jupiter Medical Center. My wife contacted him and he immediately responded and came to the hospital. Without Dr. Lubarsky's support, I don't think I would be at the health level I am at today.
I'm a big fan of Dr. Lubarsky! After moving from New York, I researched area Internist throughout Jupiter and Palm Beach Gardens. Dr. Lubarsky was a home run!