Understanding Early-Onset Cancer: Why it was So Important for Kate Middleton
In a recent revelation that has captured global attention, Kate Middleton, the Princess of Wales, shared her diagnosis of cancer, spotlighting an issue that is becoming increasingly prevalent: early-onset cancer. This development not only underscores the personal battles many face, regardless of their status but also casts a light on a concerning trend noted among younger populations.
Early-Onset Cancer: A Growing Concern
Data from the American Cancer Society indicates a worrying uptick in cancer diagnoses among adults aged 18-49. This age demographic, surprisingly, is witnessing an increase in cancer cases even as the overall cancer mortality rates improve. Such statistics emphasize a pivotal shift and necessitate a broader awareness and understanding, particularly within primary care settings.
The Role of Primary Care Physicians
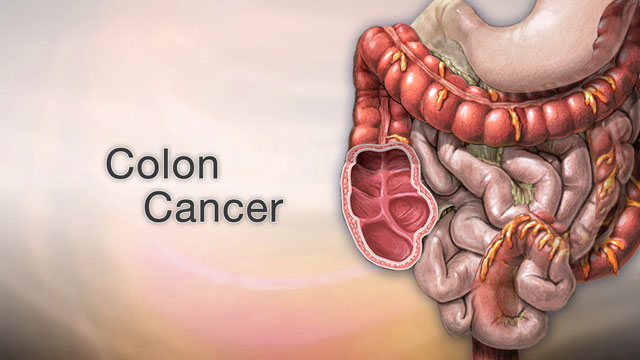
For primary care physicians, the narrative of early-onset cancer brings forth a critical responsibility. These healthcare providers are often the first line of defense, playing a pivotal role in early detection and intervention. Understanding the nuances of early-onset cancer is imperative for timely referral and management, especially given the aggressive nature of certain cancers like breast and colorectal cancer in younger patients.
Family History and Risk Assessment
A significant aspect that emerges from recent research is the role of family history in cancer risk. It is now recognized that a robust family history can be indicative of heightened cancer risk, irrespective of the cancer type within the family lineage. Primary care doctors are, therefore, encouraged to delve deeper into familial health histories, guiding patients, when necessary, to specialized high-risk clinics for further evaluation.
Addressing Younger Populations
Primary care settings must adapt to the nuances of treating younger cancer patients, who may have different needs and concerns compared to older patients. For instance, the impact of a cancer diagnosis on fertility, mental health, and lifestyle plans can be profound and requires a compassionate, tailored approach.
Awareness and Education
Finally, primary care practitioners are at the forefront of patient education. They have the unique opportunity to inform and empower their patients regarding lifestyle choices that can influence cancer risk, the importance of vaccinations (like the HPV vaccine that has impacted cervical cancer rates), and the significance of participating in recommended screening programs.
In conclusion, the news of Kate Middleton’s diagnosis is a stark reminder of cancer’s indiscriminate nature. For our primary care doctors in Jupiter, it reaffirms the importance of vigilance, early detection, and a patient-centered approach in combating the rise of early-onset cancers. By fostering awareness, advocating for regular screenings, and embracing a proactive stance, primary care doctors can significantly contribute to the early identification and management of cancer, ultimately improving outcomes for younger patients.