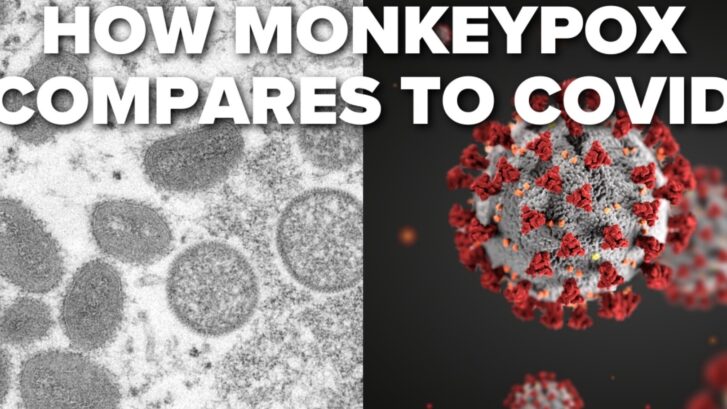
Last month, the World Health Organization (WHO) declared the newly spreading monkeypox virus a global health emergency.
This has prompted many to fear we’re heading into another coronavirus situation, as our concierge primary care doctors in Jupiter have found from talking with our patients.
While this is a debilitating, painful, and—occasionally—deadly virus, there are many reasons why it’s very dissimilar to the SARS-CoV-2 virus, the virus that causes COVID-19.
The history is different
Although both originated as “zoonotic” diseases—that it, they began in animals and spread to humans—we have a far longer history with monkeypox, meaning we know more about it than we did when the coronavirus first appeared.
According to the Centers for Disease Control and Prevention (CDC), monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, thereby giving the disease the name “monkeypox.” Its typical animal hosts, however, are rodents and other small mammals.
The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo during a period of intensified effort to eliminate smallpox. Since then, monkeypox has been reported in humans in other central and western African countries.
Although relatively new to the U.S., a large monkeypox outbreak occurred here in 2003 as a result of imported rodents.
Transmission is different
Next, the ways the two viruses are transmitted are completely different.
Unlike the largely airborne transmission of SARS-CoV-2 through aerosols that linger in the air, the monkeypox virus can only be spread through close contact with an infected person or animal, or materials such as bedding or towels that are contaminated with the virus.
In addition, monkeypox appears to be far less transmissible than COVID-19. One study found that just three percent of those in close contact with an infected person would develop monkeypox.
It appears at this time to be spreading primarily among gay and bisexual men following sexual encounters, but anyone who comes into close and prolonged, direct contact with the pox sores can become infected.
Even women, and at least two children, have been reported to have contracted monkeypox, as a result of being in close proximity to men who have sex with other men.
The symptoms are different
Unlike the stealth infections of the coronavirus, it’s very apparent when a person is infected with monkeypox. As with COVID-19 and other viruses, they develop fever, headache or body aches, chills, muscle aches, and exhaustion.
These symptoms are also similar to those of smallpox, a cousin of monkeypox, with one difference:
“A feature that distinguishes infection with monkeypox from that of smallpox is the development of swollen lymph nodes,” the CDC says.
Otherwise, however, both smallpox and monkeypox exhibit the same signature fluid-filled lesions (the so-called “pox”), which the coronavirus doesn’t produce. Some individuals have these sores all over the body, while others may have only a single lesion. This rash can be extremely painful.
The vaccines are different
When COVID-19 first appeared two-and-a-half years ago, it was a brand new virus (i.e., “novel” coronavirus).
We knew nothing about it, and at the time had no way to combat it in the form of either effective treatments or vaccines.
Because of our long history with monkeypox, however, we do have vaccines and antiviral treatments. Monkeypox and smallpox come from the same family of viruses (although monkeypox is not as severe as smallpox). That has allowed us to utilize the stockpile of smallpox vaccines and antivirals to fight monkeypox.
And, unlike the coronavirus vaccines, the vaccines for monkeypox are effective even after infection, if given within four days of exposure. Even if the vaccine is given as late as two weeks after exposure, it can still lessen the likelihood of severe illness.
Not to worry?
Does all this mean we don’t have to panic about monkeypox? Panic is never a good idea because it prevents thoughtful responses in a crisis. But at this time the monkeypox outbreak still appears to be confined largely to men who have sex with men and those who are closest to them and who may come in contact with the open sore or infected linens.
If you fall into one of those categories, it’s important to take precautions until the supply of vaccines and antivirals becomes sufficient to cover everyone at high risk of exposure, because cases are spreading rapidly in the U.S. At the end of July, the Centers for Disease Control and Prevention (CDC) reported more than 3,500 confirmed cases but noted that is probably a significant undercount.
Experts advise that, if you’re at risk, you temporarily reduce your number of sexual partners, reconsider sex with new partners, and exchange contact details with any new partners to enable follow-up, if necessary.
Infected people are encouraged to self-isolate from other humans as well as pets, and to wear a mask and long clothing over any sores.
Although there is currently a limited supply of vaccines in the U.S., the government has purchased 2.5 million doses, which should be available in the coming weeks. This means it isn’t yet enough available to offer shots to all high-risk individuals.
So until there is, take precautions, and let us know if you think your symptoms might be those of monkeypox. It’s a painful, debilitating, and sometimes deadly disease, but we can treat it if it’s caught in time.